The Leapfrog Group’s spring 2023 hospital health grades show that healthcare-associated infections are rising following the pandemic, a cause for concern for all providers. With new legislation likely on the way to Texas that will allow employers to steer their employees to steer employees toward certain hospitals within a health system, hospital quality, and safety information has never been more critical.
The risk of three healthcare-associated infections (HAI), which include staph, central line bloodstream, and catheter-associated urinary tract infections, spiked to a five-year high in hospitals during the pandemic and remains high, according to the latest Leapfrog ratings.
The results compared data from the end of 2021 and 2022 to data immediately preceding the pandemic and found that the average central line-associated bloodstream infection ratio increased by 60 percent, the staph standard infection ratio increased by 37 percent, and catheter-associated urinary tract infections standard infection ratio increased by 19 percent compared to before the pandemic.
The Centers for Disease Control had similar, if less dramatic, data about infections in the hospital. “Compared to pre-pandemic years, hospitals across the nation experienced higher than usual hospitalizations and shortages in healthcare personnel and equipment, which may have resulted in deterioration in multiple patient safety metrics since the beginning of the pandemic,” a CDC report says.
According to the latest HAI progress report, about 1 in 31 hospital patients has at least one healthcare-associated infection. In 2015, there were 687,000 HAIs in the United States, and 72,000 hospital patients with HAIs died during their hospitalizations.
“The dramatic spike in HAIs reported in this Safety Grade cycle should stop hospitals in their tracks—infections like these can be life or death for some patients,” said Leah Binder, president and CEO of The Leapfrog Group. “We recognize the tremendous strain the pandemic put on hospitals and their workforce, but alarming findings like these indicate hospitals must recommit to patient safety and build more resilience.”
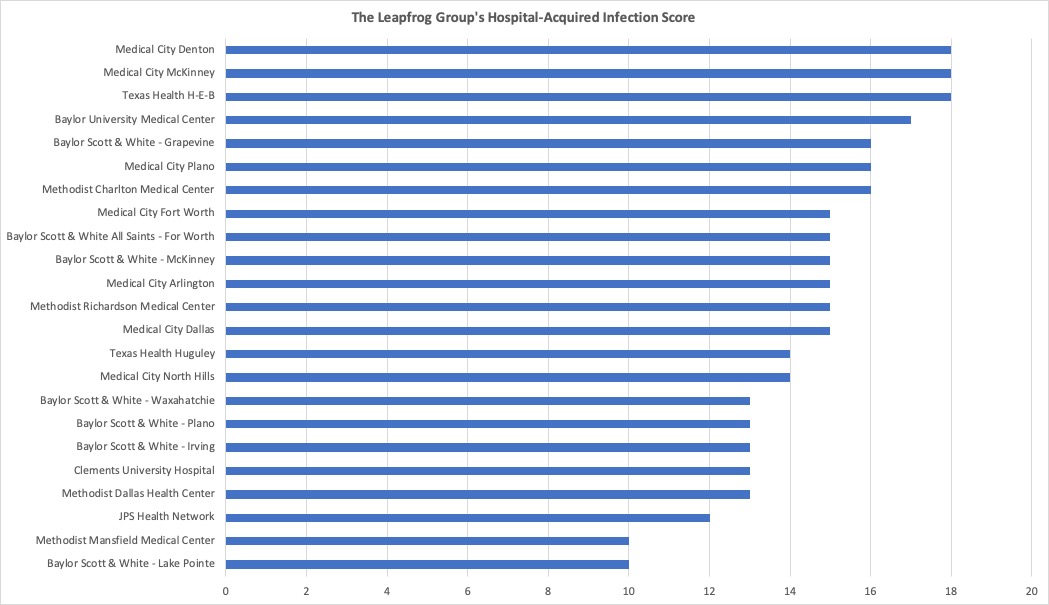
D CEO Healthcare looked at The Leapfrog Group’s ratings for North Texas Hospital’s HAIs to see how our facilities fared. Leapfrog rated each hospital for five different infections: C Diff, blood, urinary tract, MRSA (staph), and surgical site after colon surgery. We only charted the hospitals in the region that had scores for all five areas. Some hospitals only had ratings for a few infection areas, and others (Parkland Health, for one) didn’t participate in The Leapfrog Group studies at all. Each infection rating received a score from 0-4, meaning the highest score a hospital can receive is 20.
In North Texas, the Leapfrog’s top scorers were Medical City Denton, Medical City McKinney, and Texas Health Hurst-Euless-Bedford, who all received 18 points of the available 20. Baylor University Medical Center (17), Baylor Scott & White Health – Grapevine (16), and Medical City Plano (16) also scored well for HAIs.
The lowest-scoring hospitals for HAIs were Methodist Mansfield Medical Center and Baylor Scott & White Health – Lake Pointe, with just 10 points of the possible 20. Clements University Hospital, which U.S. News and World Report perennially rank as the top hospital in the region and one of the best in the state, received 13 points out of 20 for HAIs. The median score for the region was 15. You can explore the scores for the region’s hospital HAIs here.
Some authorities question the value of ranking hospitals’ infection scores if they don’t take into account the complexity of care provided at academic medical centers compared to community hospitals. In a survey of providers from the University of Maryland School of Medicine found that 84 percent of respondents said they believed hospitals and staff “intentionally manipulate” HAI rates publicly reported on the government’s Centers for Medicare and Medicaid Hospital Care Compare website. Federal reimbursement rates are set based on these metrics, and respondents said they felt pressure to find ways to avoid reporting HAI cases.
HAIs are the fourth leading cause of death in the United States behind heart disease, strokes, and cancer, according to Oxford Academic, and the top cause of preventable death. Resources were stretched during the pandemic, and worker shortages continue to plague healthcare facilities at every level without relief in the need for services, which may have increased infections.
“Not only are HAIs among the leading causes of death in the U.S., they also increase the length of hospitalization stays and add to costs,” Binder said. “Our pre-pandemic data showed improved HAI measures, but the spring 2023 Safety Grade data spotlights how hospital responses to the pandemic led to a decline in patient safety and HAI management.”
Get the D CEO Healthcare Newsletter
Author